The most common type of abdominal hernia is an inguinal or groin hernia. Patients
usually bring these hernias to the attention of their physicians when they either feel a lump in their groin or develop pain
or soreness with certain activities. The activities that
tend to exacerbate hernia pain include prolonged standing, lifting, and straining to have a bowel movement. Hernias are
essentially holes in the abdominal wall through which abdominal organs can protrude through causing a bulge or lump when looking
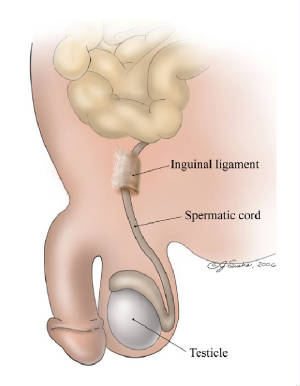
at the skin. During in uterine development, the testes descend out of the abdomen into the scrotum. They pass out of the abdominal
cavity into the inguinal canal via the deep (internal) ring and then into the scrotum via the superficial (external) ring.
In females, the same tract develops as well. This tract normally withers and disappears. In some adults, the path they take
remains and is called the processus vaginalis. In adult life, the processus vaginalis allows abdominal organs such as the
intestine, bladder, or intraabdominal fat to migrate through the abdominal wall. This is known as an indirect inguinal
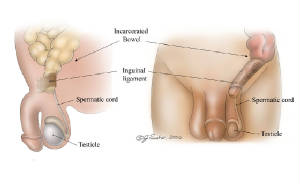
hernia. A direct inguinal hernia does not go through the inguinal canal but directly through the abdominal wall and
develops in men via wear and tear of the abdominal wall from older age or from excessive activity. Intra-abdominal contents
bulge directly out of the abdominal wall.Indirect inguinal
hernias are more common than direct inguinal hernias overall.
Who is at risk?
Hernias
occur in males much more often than they do in women. In most cases, they are congenital (present at birth). In other cases,
hernias develop from abdominal weakness due to advanced age or from excessive activity such as heavy lifting or straining.
How is it diagnosed?
Often times the hernia can be diagnosed on the basis of physical examination
as a bulge or lump on the surface of the skin that goes in and out. Some surgeons will obtain a CAT scan of the abdomen if
no hernia is felt on examination in a person with symptoms suggestive of a hernia.
Indications for Surgery
Because
of the risk of an intrabdominal organ being permanently trapped in the hernia hole instead of sliding in and out, the current
recommendation is to repair the hernia once it is recognized even if it is not causing any symptoms. There is some recent
literature, however, to suggest that watchful waiting is also an appropriate tactic to take in patients with little or mild
symptoms.
Since the diagnosis of hernia is
usually made easily on the basis of physical examination, few surgeons advocate the need for any additional imaging prior
to operation. Based on age and other pre-existing medical conditions, blood work and/or an EKG may be necessary.
Surgical Approaches - How is the surgery performed?
There
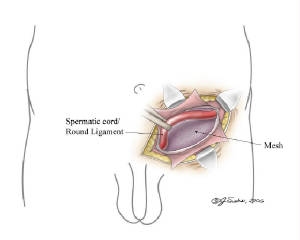
are a number of surgical approaches to hernia repair. They can be divided into two groups: open repair and the laparoscopic
repair. The most common form of open repair is the "tension-free repair" which involves the use of synthetic material
to patch over the hole. Instead of relying on the strength of weakened tissue pulled together, a piece of mesh is placed atop
the repair to create a tough scar. After shaving the skin, a straight or diagonal incision based on surgeon’s
preference is made in the groin area. The outer layer of the abdominal wall is cut to expose the inguinal canal where the
spermatic cord and blood vessels lie. In a male, the spermatic cord is identified and protected so as not to injure the vas
deferens, which is part of the spermatic cord. Once the vas deferens is identified, the search for the location of the hernia
begins. The spermatic cord is examined for the presence of a hernia sac containing abdominal organs, which would indicate
an indirect hernia. In addition, the floor of the inguinal canal a component of the abdominal wall, is examined to look for
a weakening or defect, which would indicate a direct hernia. Once the hernia is identified, any abdominal contents sticking
out of the hernia are pushed back in. The deep (internal) ring is made smaller with a mesh plug and the abdominal wall is
reinforced with an onlay mesh. The Shouldice technique, which is performed at the Shouldice clinic in Toronto, Canada does not use
any prosthetic material like the mesh. The surrounding tissues are sutured together in a special manner to completely obliterate
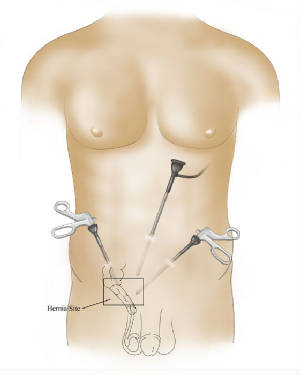
the hernia. In laparoscopic surgery, the surgery is performed with a camera called a laparoscope via an umbilical incision (i.e.
from the navel). Smaller incisions are made throughout the abdominal cavity to accommodate the other instruments needed for
the repair. Once the umbilical incision is made, the abdomen is filled with carbon dioxide gas to distend it to get a better
view of the abdominal cavity. The hernia is identified as a weakness in the abdominal wall and mesh is applied over the defect.
Because of the smaller incisions and less manipulation of the tissues, laparoscopic surgery is believed to result in less
pain and faster recovery; however some reports suggest that the recurrence rate of the hernia becomes higher.
The most common problem facing patients immediately after surgery is that of urinary retention, the inability
to pass urine. This is a side effect of the anesthesia and is usually relieved after a few hours. In some cases, if urinary
retention is prolonged, you may have a catheter inserted into your urethra. The catheter may be left in overnight and removed
in the morning. Many patients will also get tremendous swelling and bruising of the scrotum which may take a couple of weeks
to fully resolve. Hernia surgery is also typically very painful requiring regular usage of pain medicine.
It is often inadvisable for patients to return back to work until at least a week has passed from surgery. Heavy lifting is
not advised for at least six weeks after surgery. The most troubling post-operative aspect of this surgery is a recurrent hernia.
The incidence is anywhere from 1-4% over a lifetime. Other very rare, but potential complications, include
nerve entrapment syndrome and ischemic orchitis. Nerve entrapment: The ilioinguinal nerve and genitofemoral nerve are two small nerves that travel with the spermatic
cord and blood vessels. In rare cases it can get trapped in the repair. Entrapment of the ilioinguinal nerve produces pain
in the groin and scrotum. Injury to the genital branch of the genitofemoral nerve can cause hypersensitivity of the groin,
scrotum and upper thigh, and can be associated with ejaculatory dysfunction. Injection of a long-acting local anesthetic along
the course of these nerves is often helpful for diagnosing and treating entrapment. Most nerve entrapment syndromes spontaneously
resolve over time however, in few cases it becomes a chronic problem which may need surgical exploration. Ischemic orchitis arises when the
blood vessels which travel through the inguinal canal are injured. This results in a painful testicle on the side of the hernia
repair. Eventually the testicle shrinks in size and becomes nonfunctional. Fertility is generally not affected as the remaining
testicle compensates for the loss of the one testicle.