Anatomy and Physiology
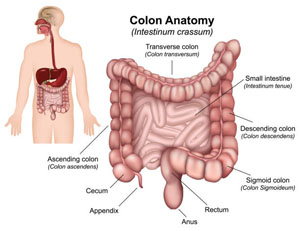
(What is the colon and what does it do?) The large bowel (colon) consists
of five main parts. The ascending colon runs from the right lower quadrant to the right upper quadrant. As it crosses over
to the left upper quadrant, it is called the transverse colon. The descending colon starts in the left upper quadrant making
its way to the left lower quadrant. The sigmoid colon is a large floppy part of the colon that connects the descending colon
to the rectum, the last part of the colon. While absorption of nutrients
mostly takes place in the small bowel, water absorption occurs in the colon. 90% of water absorption occurs in the ascending
or right colon. As the water is absorbed from stool traveling through the colon, it becomes more solid in its form. Stool
eventually comes to reside in the rectum where an urge to have a bowel movement is felt. A number of disease processes
require surgery as a potential part of therapy. A few will be discussed here. It is believed that formation
of polyps is triggered by a genetic event that causes loss of normal regulation of the growth of the mucosa, the inner lining
of the colon wall. A polyp is the end result of dysregulated growth of the mucosa. There a number of different types of polyps:
hyperplastic, hamartomas, and adenomas. While all three are benign, adenomas are pre-malignant meaning they have the potential to become cancerous. Over a number of years, adenomas have the potential to increase
in size and evolve into a cancer. Generally, the larger the adenomatous polyp, the more likely it is to be cancerous. For
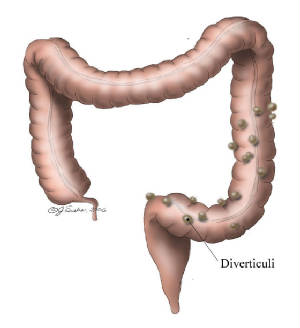
this reason, once a polyp is detected, it is removed, usually during a colonoscopy. If the polyp is too large or lays flat against the colon wall, the only method of removal is surgery. Diverticulosis is a disease characterized
by outpouchings, diverticuli, of the colon wall. There are natural areas of the weakening in the colon wall. The colon wall
can protrude outwards at these areas of weakening when the inside of the colon is subject to increased pressure. Increased
pressure can occur with constipation generally from a lack of fiber in the diet. Diverticulosis can lead to intestinal bleeding
and inflammation causing infection. In rare cases, a diverticuli can perforate leading to spillage of stool into the abdominal
cavity. 25% of people who develop a complication from diverticulosis will go on to develop another complication. If someone
suffers two or more bouts of complications diverticulosis, most physicians will recommend surgery to remove the sigmoid colon,
the part of the colon where almost all diverticuli are located.
![]()
Who is at risk? What kinds
of problems require colon surgery? How is it diagnosed? A colonoscopy is a study designed to look at the insides of the bowel. A colonoscope which is essentially a camera is inserted into
the anus and up into the bowel. If any abnormal findings are seen, biopsies can be done at the same time with small scissors
inserted through the colonoscope. In addition, most polyps can be removed during a colonoscopy as well. A barium enema is another study
formed to look at the shape of the bowel. Contrast is inserted via the anus and multiple xrays are taken as the contrast travels
from the anus up into the bowel.
How do you
prepare for surgery? Since the bowel must be divided from other
parts of the bowel to be removed, stool can leak out when the bowel is cut. The presence of stool can also impair healing
where the bowel is reconnected. For this reason, most surgeons will recommend that patients take a bowel prep to clean out
the bowels before surgery. Bowel preps include Go-lytely, Magnesium citrate, or enemas. You will probably be asked to restrict
your diet to clear liquids anywhere from 1 to 3 days before surgery. Blood
work, a chest xray, and possibly an EKG may also be required before surgery. Surgery to the colon is generally approached
by a longitudinal incision in the middle of the abdomen. Once the incision is made, the bowel is separated from its attachment
to the abdominal wall. The abnormality is identified and the bowel is divided. In performing a sigmoid colectomy, the bowel
is divided where the left colon meets the sigmoid and where the sigmoid meets the rectum. The segment of colon is removed.
The left colon is then re-connected to the rectum.
Surgical Procedure
When performing a
colectomy, for cancer, a polyp or diverticulosis, the part of the colon removed is dictated by location of the disease. The
first four segments of the colon each have one main blood vessel and chain of lymph nodes delivering blood to that segment,
so a whole segment must be removed at a time. If a mass is located somewhere in the left colon, the entire left colon is removed
as opposed to just a piece of it. So in terms of colectomy, one talks in terms of right hemicolectomies, transverse colectomies,
left hemicolectomies, sigmoid colectomy and rectal surgery.
In some special circumstances, the bowel can not be reconnected to another piece of bowel and it
is instead brought out to the skin so that stool can be emptied into a bag. This is called a colostomy. This most often happens
in emergent cases where a bowel prep could not be performed. Colostomies can be reversed, i.e. taken down so that a proper
bowel to bowel re-connection can be performed. Most surgeons wait a minimum of 6 weeks and sometimes as long as 3 months before
reversing the colostomy to allow for proper healing from the first surgery and to minimize scarring and inflammation from
the initial operation. After surgery, you will not be allowed to
eat or drink anything. When the bowels are manipulated, they become stunned for a period of time lasting between 3-5 days.
If you put anything into your bowels by eating, you will likely vomit. Approximately 3 to 5 days after surgery, your bowels
"wake up" and start moving fluid and air through. Signals that your bowels are waking up after surgery include passing
gas and having a bowel movement. Many patients are surprised to hear that they may have a bowel movement after surgery despite
the fact that they have not been eating. The bowel continues to make digestive juices which are expelled from your body as
watery bowel movements. Bowel movements after surgery will often not be of completely normal caliber until about a week to
two weeks after surgery. Once you start to pass gas or have a bowel movement, you will generally be started on clear liquids
and then given solid food. Discharge from the hospital quickly follows the introduction of solid foods into your diet.
Risks of Surgery
The biggest risk of colon surgery is a leak. This occurs when
the bowel re-connection does not heal. When the connection breaks down, stool can leak out of the colon into the abdominal
cavity causing an infection. A leak can be handled in a number of different ways. If a serious infection ensues, it will often
require a second trip to the operating room to wash out the infection, possibly disconnect the bowel and create an ostomy.
In some cases, a drain can be placed from the skin into the infection by radiology. Other risks of surgery include a small bowel obstruction. Scar tissue often forms after
surgery. When the scar tissue entraps a piece of floating small bowel, it causes a blockage. 2/3rds of the time, with complete
bowel rest and bowel de-compression, the bowel will unkink itself. The remaining 1/3rd of the time, an operation will be needed
to relieve the blockage. Some minor risks of colon surgery include
urinary tract infection, wound infection, and pneumonia.
What
to expect after surgery?
After surgery,
you will most likely wake up with a tube in your nose which empties into the stomach, a catheter in your bladder to drain
your urine, and occasionally a drain in your abdomen which emerges from your skin. The tube in your nose will probably of the three give you the
most discomfort. It is generally removed between 1-3 days after surgery.